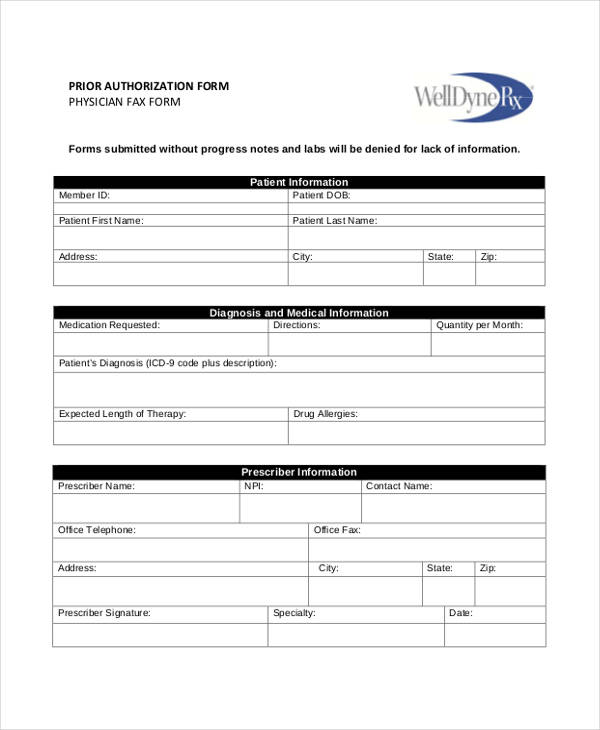
Carolina Complete Health Prior Authorization Form - This tip sheet serves as an outline to the prior authorization form. Carolina complete health medicaid face sheets. Payment of claims is dependent on eligibility, covered benefits, provider contracts, correct coding and billing practices. Web welcome to the carolina complete health page. The documents below have been designed to help radmd users navigate the prior authorization process for each program evolent (formerly national imaging associates, inc.) is responsible for. For additional information, please reference page 2 “instruction for completion” on the prior authorization form. (833) 404 2393 pharmacy pa call center: Web fax this form to: Carolinacompletehealth.com/priorauthtool submit prior authorization if a service requires authorization, submit via one of the following ways: You can access the prior authorization form, by clicking here.
For additional information, please reference page 2 “instruction for completion” on the prior authorization form. Payment of claims is dependent on eligibility, covered benefits, provider contracts, correct coding and billing practices. However, this does not guarantee payment. Carolinacompletehealth.com/priorauthtool submit prior authorization if a service requires authorization, submit via one of the following ways: This tip sheet serves as an outline to the prior authorization form. For pharmacy or medication related authorizations including: (833) 404 2393 pharmacy pa call center: Carolina complete health medicaid inpatient requests. Carolina complete health medicaid face sheets. Web welcome to the carolina complete health page. Carolina complete health medicaid assessments. You can access the prior authorization form, by clicking here. The documents below have been designed to help radmd users navigate the prior authorization process for each program evolent (formerly national imaging associates, inc.) is responsible for. Web for pharmacy prior authorization forms, please visit our pharmacy page. Web fax this form to: